Covered Services
- Can You Charge A Copay For Telemedicine
- Copay For Telemedicine
- Co Pay On Telehealth
- Bcbs Copay For Telemedicine
- Telemedicine Copay Waived
including health, dental, and pharmacy.
Virtual Mental Health Care is eligible for sharing through a teletherapy provider approved by Impact. Members must pay 100% of the session consultation fee at time of service. Consult fees are published, shared, and reimbursed (minus a $75 specialist provider fee) after the member has met their PRA.
TRICARE covers the use of secure video conferencing to provide medically necessaryTo be medically necessary means it is appropriate, reasonable, and adequate for your condition. services. You connect securely with a provider using a computer or smartphone. This includes for certain:
Medicare Part B (Medical Insurance) covers certain telehealth services. Your costs in Original Medicare. You pay 20% of the Medicare-approved amount for your doctor or other health care provider’s services, and the Part B Deductible applies. For most telehealth services, you'll pay the same amount that you would if you got the services in person. Telehealth offers patients an opportunity to connect with their care team virtually through a phone or video visit. Your care team can assess and treat medical needs, such as. Please note that there may be a co-pay associated with this visit.
- Office visits
- Preventive health screenings
- Telemental health services (individual psychotherapy, psychiatric diagnostic interviews and exams, and medication management)
- Services for End Stage Renal Disease

Using Telemedicine Services
Depending on your TRICARE plan, you may first need an authorization or referral. Contact your regional contractor. Active duty service members need a referral for telemental health care.

TRICARE recently revised its policy on telemedicine services. These changes are temporary during the national health emergency due to the pandemic. TRICARE will now:
- Cover audio-only telemedicine visits.
- Waive cost-shares and copayments for all covered telemedicine services. These services must be from a military provider or TRICARE network provider.
- Allow more providers to offer telemedicine services. Some providers may not offer this service, so be sure to ask.
- If you're overseas, the country where you live must allow telemedicine. The provider also must be licensed to practice where you live. Contact your TOP Regional Call Center for more information, including provider eligibility.
If you use TRICARE For Life, Medicare should cover telemedicine visits when the service and provider are payable by Medicare. This temporarily includes audio-only telemedicine visits. If they aren't payable by Medicare, TRICARE For Life will process as first payer. Deductibles and cost-shares will then apply. Learn more about Medicare coverage.
As of Mar. 31, 2020, TRICARE covers telehealth care for applied behavior analysis (ABA) parent or caregiver guidance services under the Autism Care Demonstration. This is an ongoing temporary change during the national health emergency due to the pandemic
Can You Charge A Copay For Telemedicine
This list of covered services is not all inclusive. TRICARE covers services that are medically necessary and considered proven. There are special rules or limits on certain services, and some services are excluded.
Last Updated 8/24/2020
Find a Doctor
Copay For Telemedicine
Prescriptions
Vision
Mental Health Therapeutic Services
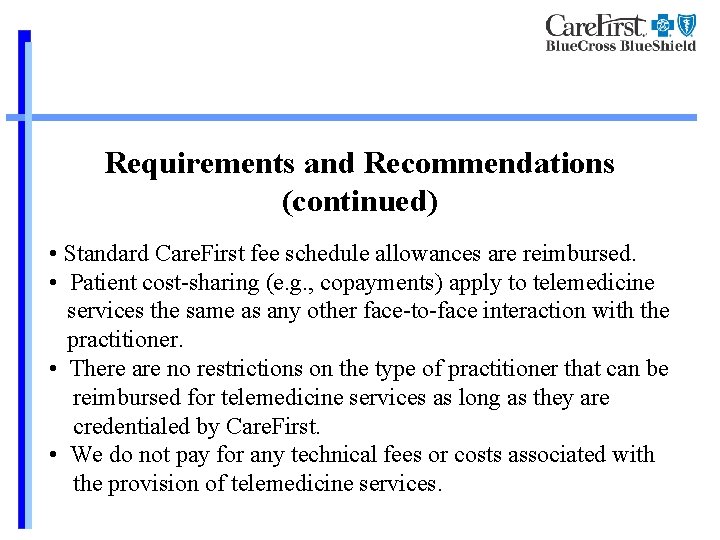
CareFirst is encouraging members to call their doctor’s office if they have symptoms of the flu, COVID-19 or other contagious conditions. During this public health event, we understand the use of telemedicine is a practical option for members who wish to or should stay home. Therefore, we have temporarily expanded our telemedicine policy. Refer to our coding guidance for all existing and temporarily covered services.
Telemedicine Capability
If your practice has its own telemedicine capability (audio/video), proceed with visits and bill CareFirst as normal with a place of service “02” and refer to this guidance for accepted telemedicine procedure codes and modifiers. Services for diagnosis, consultation or treatment provided through telemedicine must meet all the requirements of a face-to-face consultation or contact between a licensed health care provider and a patient consistent with the provider's scope of practice for services appropriately provided through telemedicine services.
If the claim is to evaluate a member for coronavirus, use diagnosis code Z20.828 (Exposure to viral disease). If you are treating a member with confirmed coronavirus use diagnosis code B97.29 for dates of service prior to 4/1/20 and diagnosis code U07.1 for dates of service on and after 4/1/20. Utilization review may be performed. Documentation in the medical record must support the services rendered.
If you are currently not set up to conduct telemedicine, you can use a commercially available platform to conduct telemedicine visits. The Office for Civil Rights (OCR) at the HHS has stated that providers may use commercially available video chat services to provide telehealth without risk that OCR might seek to impose a penalty for noncompliance with the HIPAA Rules during the COVID-19 nationwide public health emergency. Guidance and frequently asked questions can be found on their website.
Co Pay On Telehealth
Please note, CareFirst is waiving cost sharing for in-network or out-of-network visits to a provider’s office, including telemedicine, related to diagnosis and treatment of COVID-19. Providers are encouraged not to collect member cost sharing for these services. If a member does owe a copay or coinsurance after the claim is processed, you can bill the member as you do for all other claims. For these purposes we’ve defined telemedicine as a combination of interactive audio and video.
Bcbs Copay For Telemedicine
Member-Initiated Phone Consultations
CareFirst is paying for phone consultations provided by physicians and nurse practitioners credentialed in CareFirst’s network for the following specialties: primary care provider, internal medicine, OB/GYN, family practice and pediatrics. CareFirst will pay a $20 flat fee for CPT 99441.* We selected this code for all phone visits, regardless of the amount of time..

Telemedicine Copay Waived
* These benefits are covered for our fully insured members. We are also partnering closely with our self-insured customers to implement similar measures. Due to a change in D.C. law for members covered by a D.C. insured product, member-initiated phone calls are covered at $20, regardless of a provider’s specialty. Physicians and Nurse Practitioners should use CPT Codes 99441, 99442 or 99443. Non-physician providers should use CPT codes 98966, 98967 or 98968.
